- About us
- Research
- Students & Teaching
- Seminars & Events
- Directories
- Booking Rooms & Equipment
- עברית
Home » Prof. Cabantchik - Coping with iron deficiency in corona days
HOW SHOULD ONE COPE WITH IRON DEFICIENCY ANEMIA IN CORONA DAYS
Z. Ioav Cabantchik and Chaim Hershko
Institute of Life Sciences and Faculty of Medicine, Hebrew University of Jerusalem, Israel
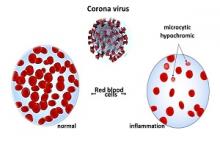
A salient feature of COVID-19 infection is a storm of cytokines that sweeps the organism and is accompanied by a rise in the serum levels of ferritin, a widely recognized acute phase reactant. As the levels of those inflammatory factors are demonstrably commensurate with the severity of the disease, they are often used as diagnostic tools to assess the disease status. However, pro-inflammatory cytokines affect body iron levels by blocking all iron gates to circulation and lead to a progressive iron-deficiency (ID) and ensuing anemia (referred as IDA). The result is depletion of circulating iron and a progressive ID that, in turn (preceding anemia), leads to increased physical weakness and major fatigue and, over time, to organ damage, especially the heart.
How does inflammation/infection affect body iron levels?
A rise in pro-inflammatory cytokines leads to a blockage of intestinal iron absorption irrespective of the iron source-animal, plant or artificial. The ensuing body iron deficit is caused by an uncompensated daily loss of 1-2 mg iron that results from the natural desquamation of death cells from tissues such as skin and gut. Moreover, the same cytokines lead also to a withdrawal of plasma iron to hepatic and splenic stores and by inducing secretion of the hormone hepcidin, to iron retention by these organs. The spleen and in some conditions also the liver recycle daily approx. 20 mg iron by digesting “old” red blood cells and secreting the iron back to circulation, commensurate with the production of new blood cells.
How does one treat ID/IDA that is refractory to oral iron supplementation?
The recommended treatment for acute ID that is refractory to oral iron has been periodic infusions of intravenous iron based on increasingly safer and more efficient formulations. The treatment is generally counter-indicated during the active phase of bacterial or viral infections. As it is applied only in clinical centers, it is also unavailable in periods of social isolation.
Alternate treatments that can substitute iv iron infusion
With the recent advent of novel iron formulations based on iron (as pyrophosphate salt) encapsulated in special lipid nanoparticle, it has become possible to use the convenient oral route to safely and effectively treat a wide variety of iron deficiencies that are refractory to oral iron supplementation. That is because some special liposomal structures can gain entry into the circulatory system (via intestinal M cells), thereby by-passing the blocked physiological entry route and enabling the supply of iron to the various organs, especially the bone marrow (for red blood cell production). The scientifically and clinically proven novel liposomal oral formulation (referred as sucrosomial iron) is a suitable and convenient alternative to intravenous iron infusions for treating a variety of ID disorders of nutritional or inflammatory origin.
How suitable are the novel iron formulations for treating ID anemia in patients with chronic disorders whos essential iv-iron supplementation is precluded due to limited clinical services?
While no iv iron supplementation is recommended during the active stages of the COVID-19 infection, patients might regain faster and improved functionalities with iron supplied by oral formulations with a proven safety and efficacy record in treating IDA in a variety of inflammatory or genetic disorders that affect body iron status. Moreover, during periods of restricted clinical services, the novel oral iron treatment can benefit the thousands of ID patients with chronic disorders that become deprived of essential iv-iron infusions.
For presentations (written material and videos of lectures) follow:
https://www.bio.huji.ac.il/sites/science.huji.ac.il/files/IOAV-REVIEW-6-8-2020_0.pdf (Hebrew);
https://www.bio.huji.ac.il/sites/science.huji.ac.il/files/IRON%20DEFICIENCY%20IN%20CORONA%20DAYS_0.pdf (English)
REFERENCES